Dr. Jill Health – OmegaPro PRM 60sg
$105.98
OmegaPro PRM features highly concentrated fish oil with a standardized quantity of the pro-resolving mediators (PRMs) 18-HEPE, 17-HDHA, and 14-HDHA. Metabolites of PRMs, known as specialized PRMs, provide building blocks to support the natural resolution of the immune response.*
Discussion
Pro-resolving mediators (PRMs) are metabolites of omega-3 and omega-6 fatty acids. The most abundant PRMs are 14-HDHA, 17-HDHA, and 18-HEPE. These PRMs are further metabolized to naturally occurring signaling molecules referred to as specialized PRMs (SPMs). The function of SPMs is to downregulate the inflammatory process after the initial immune response, allowing a return to homeostasis. Also known as “resolving agonists,” SPMs target specific immune cells to switch off, or resolve, the inflammatory response that naturally occurs with acute injury or illness.1,2 Without a resolution, inflammation may linger after the acute phase has passed, leading to an increased risk for significant chronic health issues.*1-4
Essential fatty acids are released from circulation to provide the substrate for forming SPMs. The positive benefits of omega-3s for many clinical indications may be attributed to the action of SPMs.2,5 The SPM genus is composed of the following 4 structurally distinct, prominent families of signaling molecules: lipoxins derived from arachidonic acid; resolvins derived from eicosapentaenoic acid (EPA), docosapentaenoic acid (DPA), and docosahexaenoic acid (DHA); and finally protectins and maresins derived from DPA and DHA.6,7 Each SPM has a defined structure that is pivotal to its bioaction. The endogenous biochemical SPM pathways result in counterregulation of the production of pro- inflammatory mediators (cytokines, chemokines, and inflammatory eicosanoids) to support a healthy inflammatory response.3 As a specific example, the pathways for resolvins are constituted by the fatty acid lipoxygenases and cyclooxygenase-2 via transcellular interactions generated by innate immune effector cells that migrate to inflamed tissue sites from the vasculature. Without control of this response, the activated pro-inflammatory metabolites overwhelm the tissues with persistent inflammatory cell infiltrates and edema, resulting in tissue damage.*5
Both in vitro and animal studies have demonstrated the effect of SPMs on resolution. Results of a study that explored the contribution of unresolved inflammation to heart failure after myocardial infarction in rodents found that resolvins reduced pro-fibrotic genes and collagen deposition in cardiac tissue, leading to a reduced risk of heart failure.8 In other animal research, resolvin E1 was shown to exert action on experimental models of inflammatory conditions, such as periodontitis, colitis, and peritonitis, in brain reperfusion. Resolvin E1 was also identified in the resolution of allergic airway responses. D2, another resolvin phenotype, was recognized as a regulator of the inflammatory response in mice with microbial sepsis. Additionally, the reviewers noted that the induction of macrophages resulted in a unique pro-resolving phenotype, potentially reducing the incidence of obesity-related metabolic disorders.*9
Cell culture studies have also suggested that resolvin E1 decreases polymorphonuclear neutrophil infiltration and T-cell migration, reduces TNFα and IFN-γ secretion, inhibits chemokine formation, and blocks IL-1–induced NF-κB activation. Resolvin E1 also stimulates macrophage phagocytosis of apoptotic polymorphonuclear neutrophil and is a potent modulator of pro-inflammatory leukocyte expression adhesion molecules.*1,9
An in vitro study using blood from individuals with obesity explored the hypothesis that resolution failure may lead to unrelenting inflammation in those individuals, contributing to comorbidities of obesity. The resulting data showed that leukocytes from individuals with obesity do have an unbalanced formation of SPMs regarding pro-inflammatory lipid mediators. The authors noted that supplementation of the 17-HDHA intermediate versus its DHA precursor is potentially significant for boosting impaired SPM formation when DHA metabolism is compromised, such as in obesity.*10
A randomized, double-blind crossover study in adult subjects (N = 21) assessed the response difference to EPA and DHA as precursors to SPMs. Subjects with chronic inflammation were first given 10-week supplementation with 3 g/d of EPA. After a 10-week washout period, the same subjects were supplemented with 3 g/d of DHA. The study results suggested that supplementation with EPA and DHA have distinct effects on ex vivo monocyte inflammatory response by differently regulating cytokine expression. More studies are needed to confirm the mediating effects and the molecular mechanisms of different subgroups of lipid mediators on different target cell types.*7
The effect of SPMs in limiting neutrophil infiltration into inflammatory sites, enhancing phagocytosis of apoptotic cells, and promoting tissue regeneration in cell cultures and animal models of inflammation is promising.1 However, further research is needed to better understand SPM biosynthesis and tissue- and stimulus-specific molecular signatures of the resolution, to define dosages, and to determine the application of these effects in human subjects.*
OmegaPro PRM contains an enhanced marine lipid concentrate of omega-3 fatty acid ethyl esters with a standardized level of PRMs. The concentrate is a result of a proprietary fractionation method used to enrich 18-HEPE, 17-HDHA, and 14-HDHA. Metabolites of PRMs are emerging as a promising modality for providing building blocks to support the natural resolution of the immune response.*
†These statements have not been evaluated by the Food and Drug Administration. This product is not intended to diagnose, treat, cure, or prevent any disease.
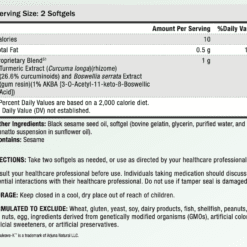
Take one softgel daily, or use as directed by your healthcare professional.
Consult your healthcare professional before use. Individuals taking blood thinners or other medication should discuss potential interactions with their healthcare professional. Do not use if tamper seal is damaged.
Only logged in customers who have purchased this product may leave a review.
Related products
Herbal
Fish Oil/Omega-3
Fish Oil/Omega-3









Reviews
There are no reviews yet.